What Is Erb’s Palsy?
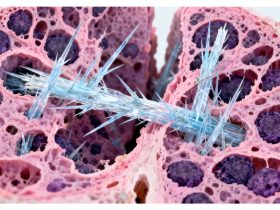
Erb’s Palsy, also known as brachial plexus palsy, is a condition that affects the nerves controlling the arm and shoulder. It happens when the brachial plexus, a network of nerves running from the spine to the shoulder, arm, and hand, gets stretched or torn. This injury typically occurs during childbirth. The severity can vary greatly, from mild weakness to complete paralysis of the arm. It’s important to recognize that Erb’s Palsy is a nerve injury, not a bone issue. The impact on an infant can range from subtle differences in arm movement to more noticeable limitations in how the arm is held or used. Understanding the basics of what Erb’s Palsy is can help parents and caregivers better support affected children. You can find more information about brachial plexus injury.
Impact of Erb’s Palsy on Infants
The way Erb’s Palsy affects a baby can be quite varied. Some infants might show very subtle signs, like a slight difference in how they move one arm compared to the other. Others may have more pronounced symptoms. Common signs to watch for include:
- A lack of movement in the affected arm or hand.
- The arm might be held in a specific position, often with the elbow straight and the arm turned inward.
- Weakness or poor muscle control in the limb.
- Reduced reflexes in the affected arm.
Early recognition of these signs is key for starting appropriate interventions. The long-term impact depends heavily on the extent of the nerve damage and how quickly treatment begins. It’s not uncommon for parents to notice these differences within the first few days or weeks of their baby’s life. If you suspect your baby might have Erb’s Palsy, it’s best to consult with a medical professional for a proper diagnosis and guidance on key signs to look for.
Causes of Erb’s Palsy
Birth Trauma and Erb’s Palsy
Erb’s Palsy most often happens because of issues during birth. A common cause is shoulder dystocia, a situation where a baby’s shoulder gets stuck behind the mother’s pelvic bone as they are being born. This can put a lot of strain on the baby’s neck and shoulder area. If doctors or midwives don’t handle this situation correctly, or if there’s a delay in helping the baby get free, the nerves in the shoulder can get stretched or torn. This kind of nerve damage is what leads to Erb’s Palsy. It’s a type of obstetric brachial plexus disorder, meaning it’s related to damage to the nerves that control the arm, which happens during childbirth [ba45].
Risk Factors During Pregnancy and Delivery
Several things can increase the chance of Erb’s Palsy happening. For instance, if the baby is unusually large (macrosomia), it can make delivery more difficult and raise the risk of shoulder dystocia. Mothers who have diabetes might also have larger babies. The way the baby is positioned in the womb can also play a role. Breech presentation, where the baby is positioned feet-first instead of head-first, can sometimes lead to a more complicated delivery. Additionally, how long labor lasts and the specific methods used during delivery, like the use of forceps or vacuum extraction, can also contribute to the risk of nerve injury. Prompt and appropriate medical care during a difficult birth is key to minimizing the chances of this happening [4103].
Recognizing Erb’s Palsy Symptoms
Recognizing Erb’s Palsy Symptoms
Common Signs in Newborns
When a baby has Erb’s palsy, it often becomes apparent shortly after birth. The most noticeable sign is how the infant uses their affected arm. Parents might observe that their baby favors one arm over the other, or that one arm appears limp and unresponsive. This can manifest in several ways:
- The baby may not move their upper arm, forearm, or hand on the affected side.
- The arm might hang limply at the baby’s side.
- The elbow may be extended, and the wrist bent.
- There could be a lack of muscle tone in the arm, making it feel floppy.
It’s important to note that these symptoms can vary in severity. Sometimes, the issue might be subtle, like a reduced range of motion in the shoulder or elbow. If you notice any of these signs, it’s a good idea to discuss them with your pediatrician. Early detection is key for managing Erb’s Palsy.
Long-Term Symptom Progression
If left unaddressed, the symptoms of Erb’s palsy can continue to affect a child as they grow. While some infants experience significant improvement with early intervention, others may face ongoing challenges. The long-term effects can include:
- Muscle weakness or atrophy (wasting) in the affected arm and hand.
- Limited range of motion in the shoulder, elbow, or wrist.
- Difficulty with fine motor skills, such as grasping objects or writing.
- Potential differences in arm length or bone development over time.
It’s not uncommon for children with Erb’s palsy to require ongoing therapy to help them develop strength and coordination. The progression of symptoms really depends on the extent of the nerve damage and the effectiveness of the treatment plan. Understanding the potential long-term outlook can help families prepare for the journey ahead and seek appropriate support, including specialized physical therapy.
Diagnosis and Medical Evaluation
Figuring out if a baby has Erb’s Palsy usually starts with a good look and some questions. Doctors will check the baby’s arms and shoulders, seeing how they move and if they feel things properly. They’ll be looking for signs like one arm hanging limp or not moving as much as the other. A key part of the diagnosis involves assessing the extent of the nerve damage. This helps everyone understand what’s going on and plan the next steps.
Diagnostic Procedures for Erb’s Palsy
When doctors suspect Erb’s Palsy, they’ll do a few things to confirm it and see how bad it is. This often includes:
- Physical Examination: A thorough check of the baby’s limbs, looking at muscle strength, reflexes, and range of motion. They’ll compare both sides of the body.
- Medical History Review: Gathering information about the birth, including any complications or difficult labor that might have led to the injury. Sometimes, injuries like this can be mistaken for other issues, like a broken collarbone, as happened with Ashton after his difficult birth [672d].
- Imaging Tests: While not always needed immediately, tests like X-rays might be used to rule out bone fractures. More advanced tests like an MRI or CT scan can provide detailed pictures of the nerves and surrounding tissues, helping to pinpoint the exact location and severity of the damage.
Assessing Nerve Damage Severity
Understanding the severity of the nerve damage is really important for treatment. Doctors use a few ways to figure this out:
- Clinical Assessment: This involves observing the baby’s movements and muscle function over time. Doctors look for specific patterns of weakness or paralysis.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests measure how well the nerves are sending signals and how the muscles are responding. They can help identify which nerves are affected and the degree of damage. These tests are usually done when the baby is a bit older.
- Grading Systems: Medical professionals often use established grading systems to classify the severity of brachial plexus injuries, which helps in tracking progress and planning treatment. Erb’s Palsy is a type of brachial plexus injury affecting nerves near the neck that control arm movement and feeling [39e5].
Treatment Strategies for Erb’s Palsy
When a baby is diagnosed with Erb’s Palsy, the focus shifts to managing the condition and helping the child regain as much function as possible. Treatment plans are usually tailored to the specific nerves affected and the severity of the damage. It’s a process that often involves a team of medical professionals working together.
Non-Surgical Interventions
Many cases of Erb’s Palsy can see significant improvement with non-surgical methods. These approaches aim to support nerve recovery and prevent complications.
- Physical Therapy: This is a cornerstone of treatment. Therapists work with the infant to perform specific exercises designed to maintain range of motion in the affected arm and shoulder. This helps prevent stiffness and contractures. Early and consistent therapy is key.
- Occupational Therapy: This type of therapy focuses on helping the child develop skills for daily activities, like feeding, dressing, and playing. It can involve adaptive equipment and strategies to make tasks easier.
- Splinting: Sometimes, splints are used to position the arm correctly, which can help protect the nerves and support healing. These are often used in conjunction with therapy.
Surgical Repair Options
For more severe nerve damage, surgery might be recommended. This is typically considered if there isn’t enough improvement with non-surgical treatments.
- Nerve Grafting: In this procedure, a surgeon takes a healthy nerve from another part of the body and uses it to bridge the gap where the original nerve was damaged. This can help re-establish a connection for nerve signals.
- Nerve Transfers: This involves rerouting a functioning nerve to take over the job of the damaged nerve. It’s another way to try and restore movement and sensation.
- Tendon Transfers: If nerve repair isn’t successful or possible, surgeons might move tendons to help restore some function to the arm or hand. This can improve movement patterns.
Therapeutic Approaches
Beyond the direct interventions, a supportive therapeutic environment is vital.
- Early Intervention Programs: Getting started with specialized programs soon after diagnosis can make a big difference. These programs often coordinate various therapies and provide resources for families.
- Monitoring and Re-evaluation: Regular check-ups with specialists are important to track progress and adjust the treatment plan as needed. The child’s development is closely watched.
- Support for Families: Dealing with a diagnosis like Erb’s Palsy can be overwhelming. Connecting with support groups and understanding the long-term outlook are important parts of the journey. Learning about options for managing cerebral palsy can also provide helpful insights into comprehensive care strategies. The goal is always to maximize the child’s potential and quality of life through consistent physiotherapy and other interventions.
Living with Erb’s Palsy
Support Systems for Families
Caring for a child with Erb’s Palsy can bring unique challenges, and finding a strong support network is really important. Many families find comfort and practical advice by connecting with others who have similar experiences. Online communities and local groups can be a great place to share stories, ask questions, and get emotional backing. These connections help families feel less alone and more equipped to handle daily life. It’s about building a community that understands the journey. You can find many helpful resources for families affected by conditions like Erb’s Palsy through organizations dedicated to supporting children with disabilities online and virtual support groups.
Long-Term Outlook and Management
The long-term outlook for children with Erb’s Palsy varies depending on the severity of the nerve damage and the effectiveness of early treatment. Many children achieve significant recovery, especially with consistent therapy and appropriate medical care. However, some may experience lasting effects that require ongoing management. This can include continued physical or occupational therapy, adaptive equipment, and regular check-ups with specialists. The goal is to help the child reach their fullest potential and maintain a good quality of life. Planning for the future, including educational support and potential career paths, is also a key part of managing Erb’s Palsy over the long term. Families can provide a fulfilling life for a child with these conditions through careful planning and accessing the right resources proper medical care.